Abstract
Introduction
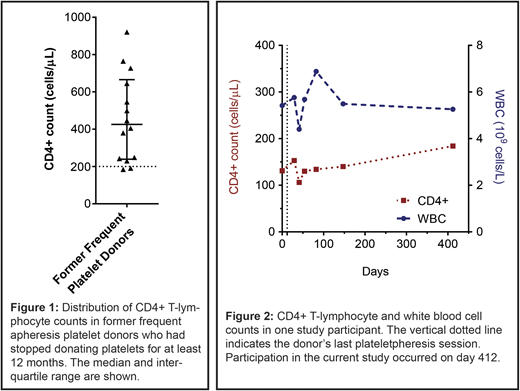
We recently discovered that a number of frequent apheresis platelet donors at our donor center had CD4+ T-lymphocyte counts below 200 cells/µL. The cause appears to be repeated extraction of these cells by the Trima Accel Automated Blood Collection System's leukoreduction system chamber. Plateletpheresis at our donor center has been conducted exclusively with this instrument since 2006. How long CD4+ T-cell lymphopenia persists after stopping plateletpheresis is unknown. Whether there are infectious or other complications that could relate to CD4+ T-cell lymphopenia in former donors is also unknown. We therefore investigated the blood counts (including CD4+ T-lymphocyte counts) and medical histories of former platelet donors who had a history of frequent platelet donation but had stopped donating platelets for at least 12 months.
Methods
We mailed a questionnaire to former frequent apheresis platelet donors who had not donated platelets at our donor center for at least 12 months. Donors who replied to the questionnaire were contacted by phone to schedule a study visit. Frequent platelet donation was defined as 20-24 plateletpheresis sessions in at least one 365-day period starting in 2011. Donors who consented to participate in the study confirmed that they had not donated platelets in the prior 12 months, provided a blood sample for analysis, and completed a health questionnaire that included questions about opportunistic infections and malignancies. Medical records of these donors were also reviewed, where available. Approval for the study was obtained from the Partners HealthCare Institutional Review Board (2017P002880) and all participants provided written informed consent.
Results
Of 52 former frequent platelet donors identified as eligible to receive a questionnaire, one was known to have died of a myocardial infarction and another had requested not to receive communications from the donor center. Therefore, 50 potential study candidates were mailed a questionnaire. Twelve questionnaires were returned as undeliverable. Five potential study candidates returned the questionnaire but either declined to participate in the study or did not respond when contacted to schedule a study visit. Fourteen former frequent platelet donors elected to participate in the study after receiving the first mailing of the questionnaire. Of these 14 study participants, 6 were female and all were Caucasian. The median age was 65. The most common reason for ceasing platelet donation was a positive HLA antibody test (5 participants) followed by "low white blood cells," "heart trouble," and "inconvenience" (2 participants each). All former donors had tested negative for HIV while donating platelets. There were 2 participants with CD4+ T-lymphocyte counts below 200 cells/µL (Figure 1); one of these participants had prior CD4+ T-lymphocyte counts available for review. These showed that the CD4+ T-lymphocyte count in this former donor had improved slightly since ceasing donation one year earlier (Figure 2). Three study participants had a CD4+ T-lymphocyte count between 200 and 300 cells/µL. A review of prescription medications and medical problems did not identify an etiology for the low CD4+ T-lymphocyte counts. Responses to the health questionnaire showed that no study participant had ever had a severe infection, an infection with an unusual pathogen ("bug"), or thrush. Two former frequent platelet donors had a history of shingles, both of whom had CD4+ T-lymphocyte counts slightly below the normal range (441-2156 cells/µL) at the time of participation in the study. Five former donors had a history of cancer: Two episodes of squamous cell skin cancer (1 participant), papillary thyroid carcinoma (1 participant), glioblastoma (1 participant), basal cell skin cancer (1 participant), and squamous cell skin cancer as well as melanoma in situ (1 participant).
Conclusion
In our small cohort, there is no evidence that CD4+ T-cell lymphopenia predisposes to opportunistic infections or to malignancies classically associated with immune dysregulation. Plateletpheresis-associated CD4+ T-cell lymphopenia has improved slightly in one former frequent platelet donor a year after ceasing plateletpheresis but the count remains below 200 cells/µL. Frequent plateletpheresis involving a leukoreduction system chamber should be considered in the differential diagnosis of idiopathic CD4+ lymphopenia.
Gansner:Novimmune SA: Research Funding; UpToDate: Patents & Royalties.
Author notes
Asterisk with author names denotes non-ASH members.